Our Mission
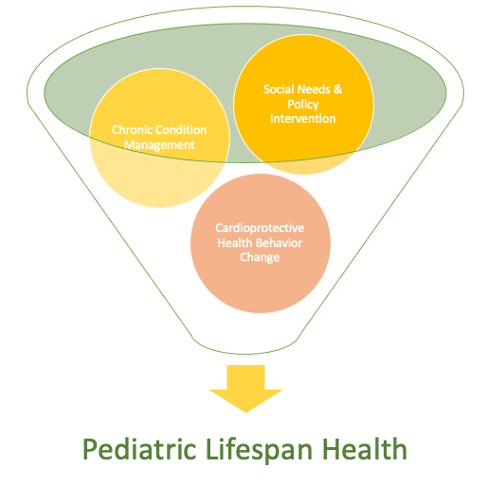
Our mission is to develop accessible and personalized interventions to improve child health outcomes. First, we collaborate with pediatric patients, families, and medical teams to design accessible interventions to promote pediatric health across development. Our interventions address three primary domains of pediatric psychology lifespan health research: chronic health condition management, cardioprotective health behavior change, and social needs/policy intervention. For example, we develop interventions that help families navigate complex care systems, adjust to managing chronic conditions, increase cardioprotective dietary choices, physical activity, and high-quality sleep, and decrease tobacco use and other health-harming behaviors, as well as address social needs like food insecurity.
Second, we personalize and optimize the delivery of our interventions by using intensive longitudinal methods to create personalized “maps” to guide intervention content and delivery. These “maps” model the interactions of biological, behavioral, social, and structural systems that contribute to a child and family’s health in daily life.
Third, we believe that success in this mission requires conducting research that centers on the lived expertise of our patients and families and speaks to the complexity of interactions between biological, behavioral, social, and structural systems in explaining health outcomes across the lifespan.
Current Projects
Developing a digital parent-teen intervention for health behavior change
Evidence-based family prevention and health behavior change programs help parents and young teens implement family practices known to reduce health-harming behavior engagement during adolescence. Evidence-based family prevention and health behavior change programs commonly target three family practices: (1) establishing and maintaining house rules; (2) increasing the frequency of parents asking and teens volunteering information about teen daily whereabouts and activities; and (3) increasing teen time spent in positive parent-teen interactions. Evidence-based family practices are shaped in these programs via extensive supported practice that is personalized to the family’s needs and social-ecological context. Unfortunately, despite well-documented efficacy, there remain substantial barriers to accessing evidence-based family prevention and behavior change programs. To bridge this access gap, we are iteratively developing and testing Parents and Teens Together (PATT), a digital parent-teen prevention program.PATT leverages a blended (virtual and health coach-led) single-session intervention for personalized instruction on evidence-based family practices and just-in-time adaptive intervention (JITAI) app technology to scale up access to personalized support for young teens and their parents to implement family practices in daily life.
- PATT Development Studies
- We are currently testing the PATT single-session intervention feasibility and acceptability and co-designing the initial JITAI prototype with families of young teens experimenting with substance use.
- Next phase: software development and a pilot micro-randomized trial to iteratively develop the PATT app. The PATT app is designed to motivate parents to ask/teens to volunteer information about the teen’s daily activities through app-based self-monitoring, a simple collaborative game in the app, and personalized reminders.
Heart health in children with chronic health conditions
Many childhood health conditions (and in some cases the treatments for those conditions) produce not only immediate risks to the child’s health but also substantially increase risk for premature cardiovascular disease (CVD) in adulthood. Prevention of premature CVD is a critical area of focus for improving health in children across the lifespan. We are collaborating with families of children with chronic health conditions that elevate risk for CVD to develop accessible interventions and models of care to improve chronic condition management, increase cardioprotective health behaviors and address social needs. In addition, our team is interested in better understanding the mechanisms by which cardiovascular health becomes interconnected with chronic disease in childhood and adolescence to help personalize and optimize the interventions we develop.
- Goal 1: Collaborative design of accessible interventions to promote lifespan health in teens with chronic health conditions that elevate risk for CVD. Next steps:
- Building community advisory boards with parents and teens (general and food insecurity)Translating our accessible diabetes intervention modules for a broader pediatric audience that includes pediatric populations designated by the AHA as having elevated risk for premature CVD (e.g., type 1 and 2 diabetes; Crohn’s, IBD, Celiac; chronic kidney and liver disease; CHD and cardiomyopathies; JIA, lupus, HIV)
- Pilot testing and refining intervention modules according to design for dissemination principles and working with dissemination stakeholders (e.g., regional pediatric cardiology team and rural school health state teams
- Goal 2: Early intervention for children with chronic health conditions that elevate risk for CVD
- We are currently collecting longitudinal data about family experiences with a fetal diagnosis of congenital heart disease.
- Next, in collaboration with families with lived experience, we are designing and testing parent-peer mentor programs to support families in navigating congenital heart disease diagnosis from birth
- We are also supporting the development of an early intervention assessment team with UVM and state partners
Past Projects
*Testing a blended digital intervention to increase physical activity in teens with type 1 diabetes
*Examining biosocial predictors of health promoting behaviors in young adults with chronic pain
*Examining self-regulation, automaticity, and diabetes management in adolescents with type 1 diabetes
*Testing a digital self-guided intervention model to improve social support, relationship health, and parenting skills in families of children recently diagnosed with type 1 diabetes
*Developing and testing a highly scalable mindfulness-based intervention as a tool for reducing diabetes distress in teens with type 1 diabetes and their families
*Exploring dynamical systems approaches to developing, testing, and evaluating adaptive and personalized public health interventions
*Examining daily self-regulatory processes that coordinate with daily blood glucose levels in teens with type 1 diabetes through electronic daily diaries
*Examining neural substrates of behavior regulation and habit formation that are associated with management of type 1 diabetes in adolescence
*Examining daily arousal, context, and substance use in adolescents that use cannabis though mobile sensing, wrist-based sensing or ecological momentary assessment
*Examining the effects of a text-based incentive program on self-regulatory capacity indexed via fMRI and increased exercise and healthy eating behaviors (via accelerometer and youth reports) in youth who have higher weight
*Examining a pilot multicomponent web-delivered intervention targeting self-regulation (via cognitive training, motivational and cognitive behavioral therapy, and incentives) and social processes (via parent training) in youth with type 1 diabetes and above-target glycemic levels